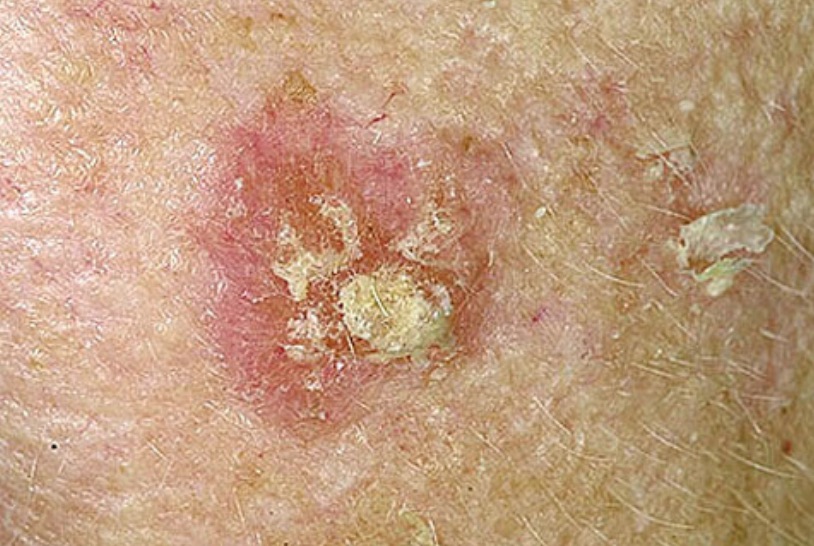
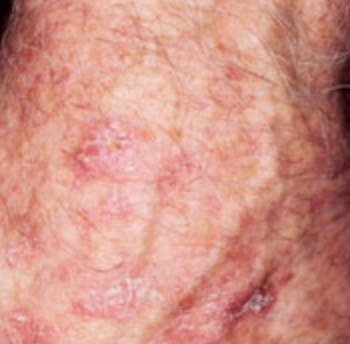
Actinic keratosis skin cancer
Actinic keratosis (pronounced ak-TIN-ik ker-uh-TOE-sis) is sometimes referred to as solar keratosis as it essentially means that it is a sun-induced change in the condition of your skin.
It is typically not something found in younger people as it develops after many years of the skin being exposed to the sun.
It will predominantly affect the back of your hands, chest, face, lips, ears, forearms, scalp and/or any areas of your body that are regularly exposed to the sun.
Actinic keratosis symptoms
The signs and symptoms look out for include:
- First signs are small, usually less than 1 inch (2.5 centimeters) in diameter, rough to the touch, as a patch of skin that is raised up from the surface of the skin
- After enlarging slowly without any additional symptoms, they become more and more raised and rough, sometimes with a hard, wart-like surface
- The rough, dry or scaly patch of skin sometimes feels as if you can peel or scratch it off
- The color is not standard at all, as it can vary from brown, grey, pink or even red, to being quite instinctive from the natural color of your skin
- There may be some itching or burning sensation in the affected area
As they are not always that visible to the naked eye or easy to see under clothing, the most common way to detect anything is therefore by feel.
As you are likely to be the one who is most familiar with your own skin, this is something you can check for very effectively by yourself.
Actinic keratosis causes and risk factors
Called the solar keratosis sometimes, it is caused by frequent, regular or intense exposure to UV rays over the years, either directly from the sun, or via tanning salons.
It will begin in the epidermis, which is the skin's outermost, top layer. Although as thin as a pencil line, it provides an excellent protective layer of skin cells that your body continually sheds and renews.
In a normal, healthy skin, the epidermis skin cells develop in a very controlled, orderly way. Healthy new cells will push older cells toward the skin's surface, where they die and are then sloughed off.
UV radiation from either sunshine or tanning lamps, that ends up damaging the skin, will actually alter the skin's texture and color, causing blotchiness and bumps or lesions. This damage adds up over the years, but only makes itself known after many years have passed.
So, the more time you spend in the sun or in a tanning booth, the greater your chance of developing any skin cancer.
Besides knowing this, there are many risk factors that you can become aware of and choose to take extra sun protection precautions:
- A skin type one does not manage easily in the sun:
pale, fair skin
blue, green or light colored eyes
blond or red hair
a tendency to freckle or burn when exposed to sunlight - A suppressed immune system through:
conditions such as leukemia, TB, AIDS
having had a major organ transplant
taking of any medicines like chemotherapy - Any continued sun exposure over time
daily work that requires being outdoors in the open sunshine
daily hobbies or recreation that exposes you to the sun and the elements - Any harsh sunburns acquired early on in life, or a history of frequent or intense sun exposure or sunburn
- Being over the age of 40
- Living in a hot, sunny climate with much outdoor appeal
- Any personal history with actinic keratosis or other skin cancers
Actinic keratosis checkups and skin biopsies
 skin cancer checkup
skin cancer checkupAlthough most doctors or skin specialists tend to regard actinic keratosis as precancerous, it is actually quite difficult to distinguish between noncancerous spots and cancerous ones.
However, if a spot or lesion on your skin persists in worrying you, go and see your doctor or ask for a referral to a dermatologist.
Take heed of the following signs if your skin:
- Is painful
- Itches or burns
- Oozes or bleeds
- Becomes scaly or crusty
- Changes in size, shape, color or elevation
At any time you may wish to, you can obtain an opinion or diagnosis for a skin growth you are suspicious about. However, a skin biopsy is usually only required to ensure there is no cancer present when the suspected actinic keratosis is quite large or has become thick in appearance. This will usually be a squamous cell skin cancer.
Basically, if it is possible, you are always safer to see a skin specialist if you notice areas of persistent roughness or scaliness in areas where you have exposed your skin to the sun.
Actinic keratosis Prognosis
The actinic keratosis growths are not defined as dangerous, or in cancer terms, are considered benign.
However, because roughly 5% will develop into squamous cell skin cancers, most people, together with their skin specialists, will opt to have them removed.
Depending on how well your skins heals, at the very worst you may have some tissue scarring, and the very least have a bit of an irritating or uncomfortable time while the skin grows.
What this will do is prevent the growth of squamous cell skin cancer, which will most likely result in your having it physically removed anyway.
Sometimes it will resolve or heal on its own, or you think it has, but then returns again after exposure to the sun again. Some people just scratch or pick it off, but then find that it returns regardless and so they repeat the cycle.
Actinic Keratosis Treatment Options
Squamous cell skin cancer resulting from actinic keratosis treatment options by physical removal include:
- Electrical cautery: effectively burns the growth off
- Curettage and electrodesiccation: scraping the growth off and then using electricity to kill any remaining cancer cells
- Excision: surgically removing the growth, requiring stitches to bind and heal the skin back together
- Cryotherapy: kills the cancerous cells by freezing the growth
If the actinic keratoses has spread to such an extent that it covers a large area, the following treatments may be an option:
- Photodynamic therapy: laser treatment
- Chemical peels: a thin layer of skin is peeled off the surface of the skin
- Creams: examples are 5-fluorouracil (5-FU) and imiquimod
NB:
It must be expected that any of these type of treatments will often leave your skin in a very delicate and irritated state.
The resultant uncomfortable redness may stay for many days while your skin heals itself. During this time you need to treat your skin with extra love and care and definitely avoid the sun!
Recommended precautions:

- Wear protective clothing such as hats, long-sleeved shirts, long skirts, or pants over areas getting too much sun exposure
- Choose high-quality toxic free sunscreens. These must contain high protection for UVA and not just UVB rays and use non-toxic ingredients that preferably have added skin healing qualities
- Apply sunscreen before going out into the sun, and reapply often
- Use sunscreen day-round and year-round, including in the winter for UVA protection
- Avoid sun lamps, tanning beds, and tanning salons unless you know they are of high quality and you never allow your skin to burn





New! Comments
Have your say... please leave me a comment in the box below.